We maximize clean claims, reduce denials, and accelerate reimbursements—working inside your EHR/PM with audit-ready workflows.

Streamlined charge capture, coding checks, and payer compliance.
Proactive status checks and escalations with daily logs.
Eligibility, documentation, and payer rules handled up front.
Front-loaded accuracy (before the claim goes out)
We catch issues at the source so claims are clean on first submission: eligibility & benefits, COB, medical necessity, coding/modifiers, required attachments (notes, labs, imaging), and payer-specific forms.
Outcome: higher first-pass rate, fewer reworks, faster payments.
Denial-prevention playbooks (by payer + code family)
We maintain checklists and edit rules per payer and service line (e.g., cardiology, ortho). Each denial code maps to a standard fix, owner, and SLA.
Outcome: measurable drop in top denial categories (COB, missing info, non-covered, prior auth).
Daily production + QA tied to KPIs
Your team gets end-of-day logs and a weekly dashboard: submissions, rejections, denials by reason, TAT, FPR, DSO/A/R aging, appeal outcomes. QA samples validate accuracy of charge entry, coding, and documentation.
Outcome: clear visibility and faster course-corrections.
Flexible engagement—scale with volume
Start with a focused scope (e.g., charge→submit + A/R follow-up) and expand as needed. Add/remove FTEs month-to-month without long contracts.
Outcome: capacity that tracks to visit volume and seasonality.
Charge capture reconciliation
Coding & modifier checks + claim edits
Submissions (EDI/paper) with required attachments
Payment posting → A/R → denials/appeals → reporting
Encounter/charge review against documentation
CPT/ICD-10 validation & bundling edits
Prior-auth & coverage confirmations, freq/exclusions
Same-day submission for complete charges
Work queues + portal/call/fax status checks
Holds/edits cleared; corrected claims/refixes sent
Escalations when SLAs slip; audit-ready notes
Weekly dashboards and aging reduction
New enrollments & re-credentialing
CAQH setup/attestation & maintenance
Demographic updates (TIN/NPI, locations, panels)
Expirables tracking + payer follow-ups to approval
Value Of Claim Process
Average A/R Days (DSO) Improvement
Charge-to-Submit TAT
Customer Retention
Number Of Claim Process
First Pass Clean Claims Rate
Revenue Improvement
Reduction in A/R (>90 days)
We boost healthcare income with quick, uncut reimbursements.

The team that makes medical claims painless
Managing claims is hard when accuracy, documentation, and payers all move at once. Our billing specialists front-load eligibility and documentation, scrub charges, and submit the claim correctly the first time—so cash arrives faster.
We reconcile encounters, validate coding/modifiers, attach what payers require, and file electronically. Then we work the queues daily so every claim reaches the insurer and gets fully reimbursed.
Secure claim data transmission
Safest encryption and least-privilege access protect PHI end-to-end.
Increase revenue
Higher first-pass approvals and fewer write-offs raise net collections.
Instant claim submission
Same-day charge review, payer edits, and electronic submission.
Claim follow-up & resolution
Systematic status checks, corrections, and timely appeals until paid.
When “good enough” isn’t enough, bring in specialists
We recover dollars left in edits and denials with 24/7 oversight. Commercial payers? Medicare/Medicaid? We maintain playbooks by payer and code family so the right fix happens quickly—refiles, corrected claims, or appeals with evidence.
We coordinate tightly with provider teams, so reimbursement forms (e.g., CMS-1500, UB-04) and supporting notes are complete. The result: fewer stalls, faster payments, clearer reporting.
We strictly adhere to compliance and state regulations and our certifications exhibit that well.



Our medical billing specialists are proficient with all EHR systems. We ensure the submission of clean claims, regardless of the EHR you use.






As a leading RCM partner, HBS supports hospitals and multi-site groups in all 50 states. Our teams understand payer rules by region and work directly in your EHR/PM to raise first-pass approvals and accelerate cash.
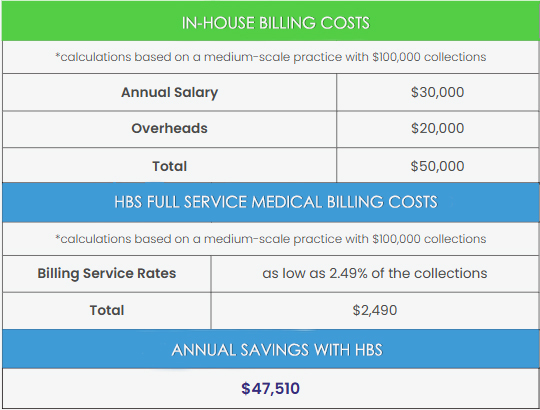
Save versus in-house billing with performance-based pricing (typically 3%–6% of monthly collections)—no setup fees, no long contracts, and a free RCM audit.
Discover what our vetted virtual medical receptionists do for hundreds of healthcare practices.
Our Success is echoed in the Satisfaction of Our Providers
"As a practice manager, I was searching for ways to streamline our medical billing process. I had tried other companies, but they were too complicated and time-consuming. Thankfully, I found HBS. They excel at customizing solutions to meet my specific needs, ."

"HBS has helped us save countless hours while significantly improving our bottom line. The team is friendly, professional, and always available to assist with any questions we have."

"HBS has helped us save time and improve the accuracy of our billing coordination. Highly recommended for any lab!"

Get in touch with us!
5550 Glades Road Suite 500-1047 Boca Raton FL 33431
Copyright 2025 Hired Billing Support LLC. All Rights Reserved.